Utilización de Riñones de Donantes con Criterios Expandidos en Brasil: Perspectivas y Recomendaciones
Palabras clave:
Trasplante de Riñón, donación de órganos, Servicios de salud, Toma de DecisionesResumen
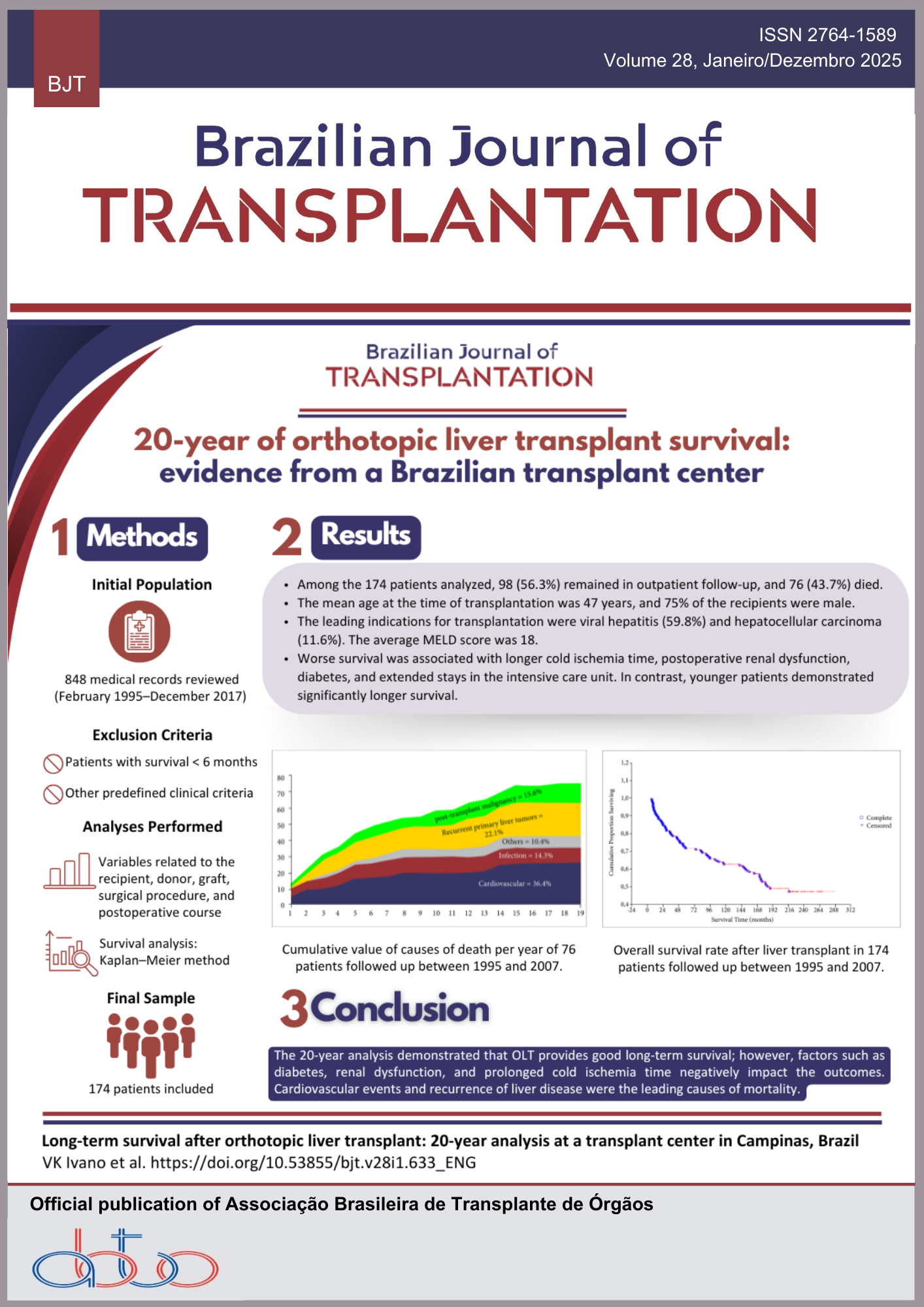
Objetivo: Investigar cómo las actitudes y el nivel de conocimiento de los profesionales de trasplante influyen en la utilización de riñones provenientes de donantes con criterios expandidos (DCE) en Brasil, e identificar acciones de gestión que puedan mejorar su uso para trasplantes.
Métodos: Estudio cualitativo basado en entrevistas semiestructuradas con 25 especialistas involucrados en el sistema de donación y trasplante de órganos en Brasil, incluyendo coordinadores, equipos de trasplante y miembros del Sistema Nacional de Trasplantes. El análisis se centró en comprender las percepciones, comportamientos profesionales y oportunidades de mejora en el uso de los riñones DCE.
Resultados: La baja utilización de riñones DCE está asociada a la falta de información, prácticas clínicas inconsistentes y percepciones de riesgo no fundamentadas en evidencia. El estudio propone recomendaciones prácticas como transparencia de datos, capacitación profesional, estandarización de procedimientos y mejora de la comunicación entre equipos.
Conclusión: La investigación ofrece aportes gerenciales y sociales al presentar acciones concretas para mejorar la eficiencia en el uso de órganos, ampliar la disponibilidad de riñones para trasplantes y salvar más vidas. También contribuye teóricamente al aplicar una perspectiva de gestión a un desafío operativo relevante en el ámbito de la salud.
Descargas
Citas
1. Almeida J, Araujo CAS, De Aguiar Roza B, Siqueira MM, Rocha E. Risk analysis of the organ donation-transplantation process in Brazil. Transplant Proc, 2021; 53(2): 607-11. https://doi.org/10.1016/j.transproceed.2021.01.018
2. Marinho A, Araújo CAS. Using data envelopment analysis and the bootstrap method to evaluate organ transplantation efficiency in Brazil. Health Care Manag Sci, 2021; 24(3): 569-81. https://link.springer.com/article/10.1007/s10729-021-09552-6
3. Andrade J, Figueiredo KF. Impact of educational and organizational initiatives in organ donation in a Southern Brazilian state in the last decade. Transplant Proc, 2019; 51(3): 625-31. https://doi.org/10.1016/j.transproceed.2018.10.033
4. Vanholder R, Domínguez-Gil B, Busic M, Cortez-Pinto H, Craig JC, Jager KJ, et al. Organ donation and transplantation: a multi-stakeholder call to action. Nat Rev Nephrol, 2021; 17(8): 554-68. https://doi.org/10.1038/s41581-021-00425-3
5. Silva SB, Caulliraux HM, Araújo CAS, Rocha E. Uma comparação dos custos do transplante renal em relação às diálises no Brasil. Cad Saude Publica, 2016; 32(6): e00013515. https://doi.org/10.1590/0102-311X00013515
6. Pérez-Sáez MJ, Montero N, Redondo-Pachón D, Crespo M, Pascual J. Survival benefit from kidney transplantation using kidneys from deceased donors aged ≥ 75 years: a time‐dependent analysis. Am J Transplant, 2016; 16(9): 2724-33. https://doi.org/10.1111/ajt.13776
7. Chaudhry D, Chaudhry A, Peracha J, Sharif A. Survival for waitlisted kidney failure patients receiving transplantation versus remaining on waiting list: systematic review and meta-analysis. BMJ, 2022; 376: e068769. https://doi.org/10.1136/bmj-2021-068769
8. Soares LSS, Brito ES, Magedanz L, França F A, Araújo WN, Galato D. Solid organ transplantation in Brazil: a descriptive study of distribution and access inequalities across the Brazilian territory, 2001-2017. Epidemiol Serv Saúde, 2020; 29(1): e2018383. https://doi.org/10.5123/S1679-49742020000100005
9. Gómez EJ, Jungmann S, Lima AS. Resource allocations and disparities in the Brazilian health care system: insights from organ transplantation services. BMC Health Serv Res, 2018; 18(1): 90. https://doi.org/10.1186/s12913-018-2851-1
10. Associação Brasileira de Transplante de Órgãos. Dimensionamento dos transplantes no Brasil e em cada estado (2015-2022). Registro Brasileiro de Transplantes. 2022; XVII (4). Disponível em: https://site.abto.org.br/wp-content/uploads/2023/03/rbt2022-naoassociado.pdf
11. Moura LC, Matos GM. Manual do núcleo de captação de órgãos: iniciando uma Comissão Intra Hospitalar de Doação de Órgãos e Tecidos para Transplantes – CIHDOTT. Barueri: Minha Editora; 2014.
12. Westphal GA, Garcia VD, Souza RL, Franke CA, Vieira KD, Birckholz VRZ, et al. Diretrizes para avaliação e validação do potencial doador de órgãos em morte encefálica. Rev Bras Ter Intensiva, 2016; 28(3): 220 55. https://doi.org/10.5935/0103-507X.20160048
13. Mota LS, Oliveira CMC, Pinheiro Junior FML, Santos LCO, Nóbrega DG, Fernandes PF, et al. Estudo comparativo entre transplantes renais com doador falecido critério expandido e critério padrão em um único centro no Brasil. J Bras Nefrol, 2016; 38(3): 334-43. https://doi.org/10.5935/0101-2800.20160051
14. Rose C, Schaeffner E, Frei U, Gill J, Gill JS. A lifetime of allograft function with kidneys from older donors. J Am Soc Nephrol, 2015; 26(10): 2483-93. https://doi.org/10.1681/asn.2014080771
15. Rijkse E Ceuppens S, Qi H, IJzermans JNM, Hesselink DA, Minnee RC. Implementation of donation after circulatory death kidney transplantation can safely enlarge the donor pool: a systematic review and meta-analysis. Int J Surg, 2021; 92: 106021. https://doi.org/10.1016/j.ijsu.2021.106021
16. Cooper M, Formica R, Friedewald J, Hirose R, O’Connor K, Mohan S, et al. Report of National Kidney Foundation Consensus Conference to decrease kidney discards. Clin Transplant, 2019; 33(1): e13419. https://doi.org/10.1111/ctr.13419
17. Ojo AO, Hanson JA, Meier-Kriesche HU, Okechukwu CN, Wolfe RA, Leichtman AB, et al. Survival in recipients of marginal cadaveric donor kidneys compared with other recipients and wait-listed transplant candidates. J Am Soc Nephrol, 2001; 12(3): 589-97. https://jasn.asnjournals.org/content/12/3/589
18. Chapman JR, O’Connell PJ, Nankivell BJ. Follow-up after renal transplantation with organs from donors after cardiac death. Transpl Int, 2006; 19(9): 715-9. https://doi.org/10.1111/j.1432-2277.2006.00341.x
19. Greenstein SM, Moore N, McDonough P, Schechner R, Tellis V. Excellent outcome using “impaired” standard criteria donors with elevated serum creatinine: outcome using “impaired” standard criteria donors with elevated serum creatinine. Clin Transplant, 2008; 22(5): 630-3. https://doi.org/10.1111/j.1399-0012.2008.00932.x
20. Klassen DK, Edwards LB, Stewart DE, Glazier AK, Orlowski JP, Berg CL. The OPTN deceased donor potential study: Implications for policy and practice. Am J Transplant, 2016; 16(6): 1707-14. https://doi.org/10.1111/ajt.13670
21. Stewart DE, Garcia VC, Aeder MI, Klassen DK. New insights into the alleged Kidney Donor Profile Index labeling effect on kidney utilization. Am J Transplant, 2017; 17(10): 2696-2704. https://doi.org/10.1111/ajt.14344
22. Snyder JJ, Salkowski N, Wey A, Israni AK, Schold JD, Segev DL, et al. Effects of high‐risk kidneys on scientific registry of transplant recipients program quality reports. Am J Transplant, 2016; 16(9): 2646-53. https://doi.org/10.1111/ajt.13793
23. Schnier KE, Fischbacher U, Scott DL. Transplantation at the nexus of behavioral economics and health care delivery: transplantation and behavioral economics. Am J Transplant, 2013; 13(1): 31-5. https://doi.org/10.1111/ajt.12028
24. Heilman RL, Green EP, Reddy KS, Moss A, Kaplan B. Potential impact of risk and loss aversion on the process of accepting kidneys for transplantation. Transplantation, 2017; 101(7): 1514-8. https://doi.org/10.1097/TP.0000000000001619
25. Kumar D, Humar A, Kim SJ, Kiberd B. A survey of increased infectious risk donor utilization in Canadian transplant programs. Transplantation, 2016; 100(2): 461-4. https://doi.org/10.1097/TP.0000000000001011
26. Deulofeu R, Bodí MA, Twose J, López P. How to achieve more accurate comparisons in organ donation activity: time to effectiveness indicators. Transplant Proc, 2010; 42(5): 1432-8. https://doi.org/10.1016/j.transproceed.2010.03.097
27. Siqueira MM, Araujo CA, De Aguiar Roza B, Schirmer J. Indicadores de eficiência no processo de doação e transplante de órgãos: revisão sistemática da literatura. Rev Panam Salud Publica, 2016; 40(2): 90-7. https://www.scielosp.org/pdf/rpsp/2016.v40n2/90-97
28. Chen SS, Pankratz VS, Litvinovich I, Al-Odat RT, Unruh ML, Ng Y-H , et al. Expanded criteria donor kidneys with kidney donor profile index ≤ 85%: are we doing enough to counsel our patients? Transplant Proc, 2020; 52(1): 54-60. https://doi.org/10.1016/j.transproceed.2019.11.005
29. Badovinac K, Greig PD, Ross H, Doig CJ, Shemie SD. Organ utilization among deceased donors in Canada, 1993-2002. Can J Anaesth, 2006; 53(8): 838-44. https://doi.org/10.1007/BF03022802
30. Lledó‐García E, Riera L, Passas J, Paredes D, Morales JM, Sánchez‐Escuredo A, et al. Spanish consensus document for acceptance and rejection of kidneys from expanded criteria donors. Clin Transplant, 2014; 28(10): 1155-66. https://doi.org/10.1111/ctr.12434
31. Sibulesky L, Gillingham KJ, Matas AJ. Changing the paradigm of organ utilization from PHS increased risk donors: an opportunity whose time has come? Clin Transplant, 2015; 29(9): 724-7. https://doi.org/10.1111/ctr.12582
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2025 Joel de Andrade, Claudia Affonso Silva Araujo, Marina Martins Siqueira, Mônica Ferreira da Silva

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.