Maribavir in the Treatment of Cytomegalovirus Infections that are Resistant and/or Refractory in Transplant Recipients
Keywords:
Antivirals, Cytomegalovirus Infections, TransplantationAbstract
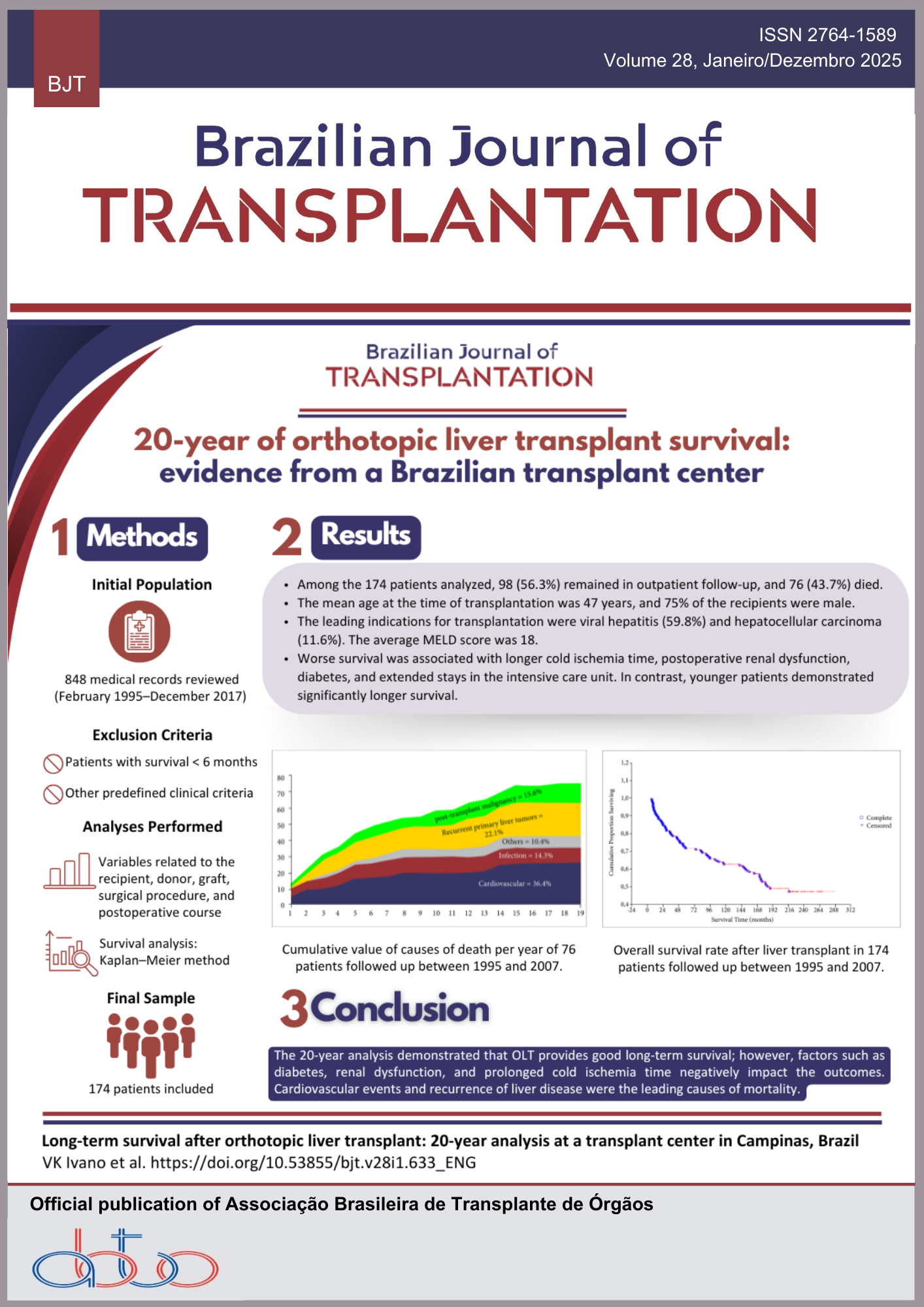
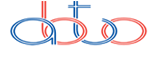
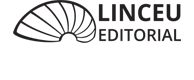
Objectives: This scoping review aims to gather data and map the available evidence on the efficacy and safety of maribavir (MBV) in transplant patients with resistant and/or refractory CMV infection. Methods: This is a scoping review conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) guidelines. The databases searched were MEDLINE, Scopus, Embase, Web of Science, and LILACS. The search used the keywords “Maribavir,” “Cytomegalovirus,” “Resistance,” and “Transplantation,” along with their synonyms and appropriate Boolean operators. Results: A total of 640 articles were retrieved in the literature search, of which 11 were included in the review. Phase 3 clinical trials showed that MBV is more effective and safer than conventional antivirals, with higher rates of viral clearance and a lower incidence of toxicities such as nephrotoxicity and myelotoxicity. Virological response rates to MBV ranged from 21% to 90%, with greater efficacy observed at week 8 compared to conventional therapies. Recurrences occurred in 20.8% to 40% of cases, mainly associated with high initial viral load. Conclusion: MBV stands out as an effective therapeutic option with a more favorable safety profile. Despite its demonstrated benefits, the emergence of resistance and viral recurrences remains an ongoing challenge. Further studies are needed to assess its impact on long-term clinical outcomes and to optimize management strategies, especially in specific patient subgroups.
Downloads
References
1. Griffiths P, Reeves M. Pathogenesis of human cytomegalovirus in the immunocompromised host. Nat Rev Microbiol, 2021; 19(12): 759-73. https://doi.org/10.1038/s41579-021-00582-z
2. Royston L, Papanicolaou GA, Neofytos D. Refractory/resistant cytomegalovirus infection in transplant recipients: an update. Viruses, 2024; 16(7): 1085. https://doi.org/10.3390/v16071085
3. Bassel M, Romanus D, Bo T, Sundberg AK, Okala S, Hirji I. Retrospective chart review of transplant recipients with cytomegalovirus infection who received maribavir in the phase 3 SOLSTICE trial: data at 52 weeks post-maribavir treatment initiation. Antivir Ther, 2023; 28(5). https://doi.org/10.1177/13596535231195431
4. Kotton CN, Kumar D, Caliendo AM, Huprikar S, Chou S, Danziger-Isakov L, et al. The Third International Consensus Guidelines on the Management of Cytomegalovirus in Solid-organ Transplantation. Transplantation, 2018; 102(6): 900-31. https://doi.org/10.1097/TP.0000000000002191
5. Green ML, Leisenring W, Pergam SA. CMV reactivation after allogeneic HCT and its effect on immune recovery and longterm outcomes. Blood, 2013; 122(7): 1316-24. https://doi.org/10.1182/blood-2013-02 487074
6. Brasil. Ministério da Saúde. Comissão Nacional de Incorporação de Tecnologias no Sistema Único de Saúde. Relatório de recomendação nº 946: Maribavir para o tratamento de citomegalovírus refratário, com ou sem resistência, em pacientes adultos pós-transplante. 2024 [accessed on May 18, 2025]. Available at: https://www.gov.br/conitec/pt-br/midias/relatorios/2024/relatorio-de-recomendacao-no-946-maribavir-para-o-tratamento-de-citomegalovirus-refratario-com-ousem-resistencia-em-pacientes-adultos-pos-transplantes/view
7. Chou S. Cytomegalovirus UL97 mutations in the era of maribavir. Reviews in Medical Virology. Rev Med Virol, 2008; 18(4): 233-46. https://doi.org/10.1002/rmv.574
8. Avery RK, Alain S, Alexander BD, Blumberg EM, Chemaly RF, Cordonnier C et al. Maribavir for refractory cytomegalovirus infections with or without resistance post-transplant: results from a phase 3 randomized clinical trial. Clin Infect Dis, 2022; 75(4): 690-701. https://doi.org/10.1093/cid/ciab988
9. Gandhi RG, Kotton CN. Evaluating the safety of maribavir for the treatment of cytomegalovirus (CMV). Ther Clin Risk Manag, 2022;18: 223-32. https://doi.org/10.2147/TCRM.S303052
10. Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMAScR): checklist and explanation. Ann Intern Med, 2018;169(7): 467-73. https://doi.org/10.7326/M18-0850
11. Pollock D, Peters MDJ, Khalil H, McInerney P, Alexander L, Tricco AC. Recommendations for the extraction, analysis, and presentation of results in scoping reviews. JBI Evid Synth, 2023; 21(3): 520-32. https://doi.org/10.11124/JBIES-22-00123
12. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan – a web and mobile app for systematic reviews. Syst Ver, 2016; 5(1): 210. https://doi.org/10.1186/s13643-016-0384-4
13. Blumberg AM, Witzke O, Harber M, Ison MG, Saliba F, Kamar N, et al. Maribavir for refractory cytomegalovirus infection (with or without resistance) in solid organ transplant recipients: subgroup analysis of the phase 3 randomized SOLSTICE study. J Heart Lung Transplant, 2025; 44(6): 986-94. https://doi.org/10.1016/j.healun.2024.11.026
14. Chou S, Alain S, Cervera C, Chemaly RF, Kotton CN, Lundgren J, et al. Drug resistance assessed in a phase 3 clinical trial of maribavir therapy for refractory or resistant cytomegalovirus infection in transplant recipients. J Infect Dis, 2024; 229(2): 413-21. https://doi.org/10.1093/infdis/jiad293
15. Papanicolaou GA, Avery KR, Cordonnier C, Duarte RF, Haider S, Maertens J. Treatment for first cytomegalovirus infection post-hematopoietic cell transplant in the AURORA Trial: a multicenter, double-blind, randomized, phase 3 trial comparing maribavir with valganciclovir. Clin Infect Dis, 2024; 78(3): 562-72. https://doi.org/10.1093/cid/ciad709
16. Chou S, Winston DJ, Avery KR, Cordonnier C, Duarte RF, Haider S, et al. Comparative emergence of maribavir and ganciclovir resistance in a randomized phase 3 clinical trial for treatment of cytomegalovirus infection. J Infect Dis, 2025; 231(3): e470-7. https://doi.org/10.1093/infdis/jiae469
17. Ni B, Wolfe CR, Arif S, Carugati M, Heldman MR, Messina JA, et al. Real-world experience with maribavir for treatment of cytomegalovirus infection in high-risk solid organ transplant recipients. Open Forum Infect Dis, 2024; 11(7): ofae335.https://doi.org/10.1093/ofid/ofae335
18. Beechar VB, Phadke VK, Pouch SM, Mehta AK, Karadkhele G, Larsen CP, et al. Evaluating real-world experience with maribavir for treatment of refractory/resistant cytomegalovirus in renal transplant recipients. Clin Transplant, 2024; 38(10): e15480. https://doi.org/10.1111/ctr.15480
19. Ogawa L, Morinishi C, Multani A, Gaynor P, Beaird OE, Pham C, et al. Real-world comparison of maribavir to foscarnet for the treatment of cytomegalovirus in solid organ and hematopoietic stem cell transplant recipients. Viruses, 2024; 16(12):1889. https://doi.org/10.3390/v16121889
20. Daher M, Khawaja F, Spallone A, Shigle TL, Bhatti M, Vuong NN, et al. Real-world experience with maribavir for treatment of refractory or resistant cytomegalovirus infection in hematopoietic cell transplant recipients and hematologic malignancy patients. Transpl Infect Dis, 2025; 27(2): e14444. https://doi.org/10.1111/tid.14444
21. Papanicolaou GA, Silveira FP, Langston AA, Pereira MR, Avery RK, Uknis M, et al. Maribavir for refractory or resistant cytomegalovirus infections in hematopoietic-cell or solid-organ transplant recipients: a randomized, dose-ranging, doubleblind, phase 2 study. Clin Infect Dis, 2019; 68(8): 1255-64. https://doi.org/10.1093/cid/ciy706
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Adla Sophia Barros da Mota , Alessandra Maria Soares de Brito, Sophia Laura de Queiroz Cabral, Mariana Brilhante da Nóbrega Dantas de Moraes, Marília de Almeida Farias Nascimento, Leonardo Amaral Vieira, Lucas Ribeiro Ferraz, Arine Maria Víveros de Castro Lyra, Lillian Christyne de Oliveira Arruda, Hugo Rafael de Souza e Silva

This work is licensed under a Creative Commons Attribution 4.0 International License.