Long-Term Quality of Life of Kidney Transplant Recipients
Keywords:
Qualidade de Vida, Transplante, Doador, Cadáver, RenalAbstract
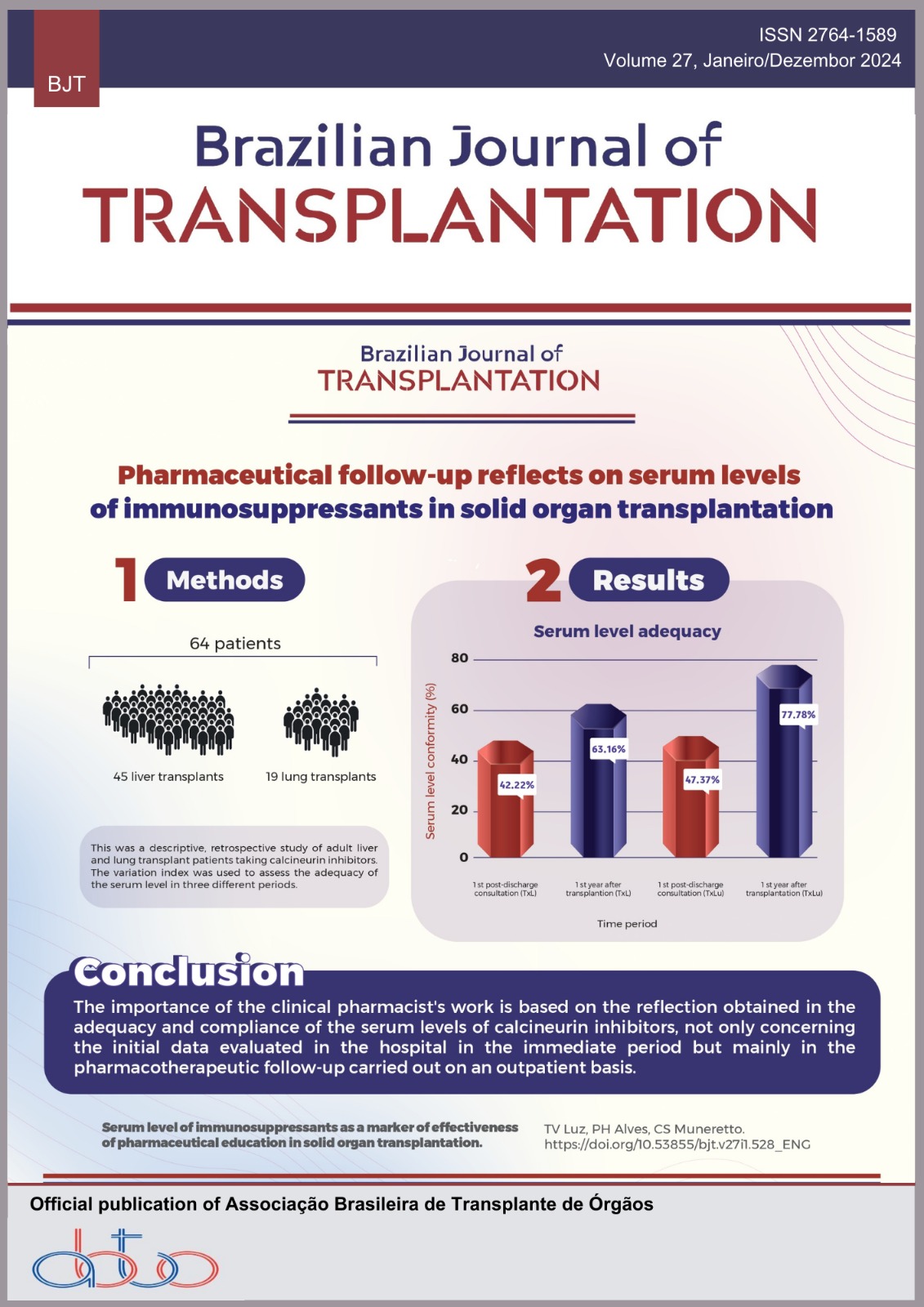
Introduction: The relevance of quality of life is increasingly evident in rising life expectancy and the prevalence of noncommunicable chronic diseases like chronic kidney disease. Transplantation is the preferred treatment for end-stage chronic kidney disease, facilitated through living or cadaveric donors as per Brazilian legislation. However, limited literature compares long-term quality of life data and its correlation with graft origin. This study addresses this knowledge gap, focusing on patients who underwent kidney transplantation before 2012 at Hospital Universitário Evangélico Mackenzie. Objectives: The primary aim is to analyze kidney transplant recipients’ long-term quality of life from living and cadaveric donors. Methods: The study was observational cross-sectional; the sample includes 24 female (61.5% cadaveric donor) and 19 male (38.5% cadaveric donor) patients who underwent transplantation before 2012. The Short Form-36 (SF-36) questionnaire was utilized, and data were statistically analyzed after tabulation in Excel®. Results: Cadaveric donor recipients experienced 39 additional months of dialysis (p = 0.017) and higher initial median creatinine levels than living donor recipients. Creatinine findings were morefavorable for living donor recipients in the 7th and 8th years, indicating a temporal decline in the cadaveric donor group. In the SF-36 questionnaire, only the “mental health” domain showed a statistically significant difference, favoring the cadaveric donor group (p = 0.008). Conclusion: Long-term quality of life for living donor and cadaveric donor kidney transplant recipients did not significantly differ, except for the “mental health” domain, which favored cadaveric donor recipients. Creatinine levels exhibited a temporal decline in the cadaveric donor group, emphasizing the importance of considering graft origin in assessing transplant outcomes.
Downloads
References
BRASIL. Ministério da Saúde. Diretrizes clínicas para o cuidado ao paciente com doença renal crônica no Sistema Único de Saúde. Brasília (DF): Ministério da Saúde; 2014.
Romão Junior JE. Doença renal crônica: definição epidemiologia e classificação. J Bras Nefrol. 2004 [access on 08 Jan 2022]; 26(3):1-3. Available at: https://www.bjnephrology.org/article/doenca-renal-cronica-definicao-epidemiologia-eclassificacao/
Cherchiglia ML, Machado EL, Szuster DAC, Andrade EIG, Acúrcio F de A, Caiaffa WT, et al. Perfil epidemiológico dos pacientes em terapia renal substitutiva no Brasil, 2000-2004. Rev Saude Publica. 2010 [access on 10 Jan 2022];44(4):639-49. Available at: https://www.scielosp.org/pdf/rsp/2010.v44n4/639-649/pt
Costa JM, Nogueira LT. Association between work, income and quality of life of kidney transplant recipient the municipality of Teresina, PI, Brazil. Braz J Nephrol 2014;36(3):332-8. https://doi.org/10.5935/0101-2800.20140048
Santos LF, Prado B da C, Castro FP dos S, Brito RF, Maciel SC, Avelar TC. Qualidade de vida em transplantados renais. Psico-US. 2018;23(1). https://doi.org/10.1590/1413-82712018230114
Pedro HA . Anexos.pdf. figshare. Online resource 2024. https://doi.org/10.6084/m9.figshare.26029540.v1
Chen TK, Knicely DH, Grams ME. Chronic kidney disease diagnosis and management: a review. JAMA 2019;322(13):1294- 1304. https://doi.org/10.1001/jama.2019.14745
Machado EL, Caiaffa WT, César CC, Gomes IC, Andrade EIG, Acúrcio F de A, et al. Iniquities in the access to renal transplant for patients with end-stage chronic renal disease in Brazil. Cad Saude Publica 2011;27Suppl 2):s284-97.
Fraser WD. Hyperparathyroidism. Lancet 2009;374(9684):145-58. https://doi.org/10.1016/S0140-6736(09)60507-9
Karam VH, Gasquet I, Delvart V, Hiesse C, Dorent R, Danet C, et al. Quality of life in adult survivors beyond 10 years after liver, kidney, and heart transplantation. Transplantation 2003;76(12):1699-704. https://doi.org/10.1097/01.TP.0000092955.28529.1E
Kim GH, Park TH, Choi JY, Lim JH, Jung HY, Choi JY, et al. Analysis of clinical outcomes according to the definition of slow graft function in deceased donor kidney transplantation. Transplant Proc 2019;51(8):2587-92. https://doi.org/10.1016/j.transproceed.2019.03.066
Valdivia MAP, Gentil MA, Toro M, Cabello M, Rodríguez-Benot A, Mazuecos A, et al. Impact of cold ischemia time on initial graft function and survival rates in renal transplants from deceased donors performed in Andalusia. Transplant Proc 2011;43(6):2174-6. https://doi.org/10.1016/j.transproceed.2011.06.047
Yazdani B, Marinez J, Krüger B, Kälsch AI, Jung M, Chen G, et al. Patient and graft survival after dual kidney transplantation with marginal donors in comparison to matched control groups. Transplant Proc 2021;53(7):2180-7. https://doi.org/10.1016/j.transproceed.2021.07.016
Kim DW, Tsapepas D, King KL, Husain SA, Corvino FA, Dillon A, et al. Financial impact of delayed graft function in kidney transplantation. Clin Transplant 2020;34(10):e14022. https://doi.org/10.1111/ctr.14022
Yemini R, Rahamimov R, Ghinea R, Mor E. Long-term results of kidney transplantation in the elderly: comparison between different donor settings. J Clin Med 2022;10(22):5308. http://doi.org/10.3390/jcm10225308
Pehlivan S, Vatansever N, Arslan İ, Yildiz A, Ersoy A. Level of daily life activities and learning needs in renal transplant patients. Experimental and Clinical Transplantation 2020;18(4):498-504. https://doi.org/10.6002/ect.2018.0151
Woźniak I, Kolonko A, Chudek J, Nowak, Farnik M, Więcek A. Influence of polypharmacy on the quality of life in stable kidney transplant recipients. Transplant Proc 2018;50(6):1896-9. https://doi.org/10.1016/j.transproceed.2018.02.128
Mouelhi Y, Jouve E, Alessandrini M, Pedinielli N, Moal V, Meurette A, et al. Factors associated with health-related quality of life in kidney transplant recipients in France. BMC Nephrol 2018;19:99. https://doi.org/10.1186/s12882-018-0893-6
Sharif A, Baboolal K. Complications associated with new-onset diabetes after kidney transplantation. Nat Rev Nephrol 2011;8(1):34-42. https://doi.org/10.1038/nrneph.2011.174
Milaniak I, Rużyczka EW, Dębska G, Król B, Wierzbicki K, Tomaszek L, et al. Level of life quality in heart and kidney transplant recipients: a multicenter study. Transplant Proc 2020;52(7):2081-6. https://doi.org/10.1016/j.transproceed.2020.03.038
Laguardia J, Campos MR, Travassos C, Najar AL, dos Anjos LA, Vasconcellos MM. Dados normativos brasileiros do questionário Short Form-36 versão 2. Rev Bras Epidemiol 2013;16(4):889-97. https://doi.org/10.1590/S1415-790X2013000400009
National Institutes of Health. NIDDK USRDS. Annual data report.2021. [access on 3May 2022]. Available at: https://adr.usrds.org/2021/end-stage-renal-disease/7-transplantation
Ravagnani LMB, Domingos NAM, Miyazaki MC de OS. Qualidade de vida e estratégias de enfrentamento em pacientes submetidos a transplante renal. Estud Psicol (Natal) 2007;12(2). https://doi.org/10.1590/S1413-294X2007000200010
Lee D, Kanellis J, Mulley WR. Allocation of deceased donor kidneys: a review of international practices. Nephrology 2019; 24(6):591-8. https://doi.org/10.1111/nep.13548
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Renata Namie Yoshioka Kimura, Pedro Henrique Haisi Amaral Camargo, Paulo Eduardo Dietrich Jaworski

This work is licensed under a Creative Commons Attribution 4.0 International License.