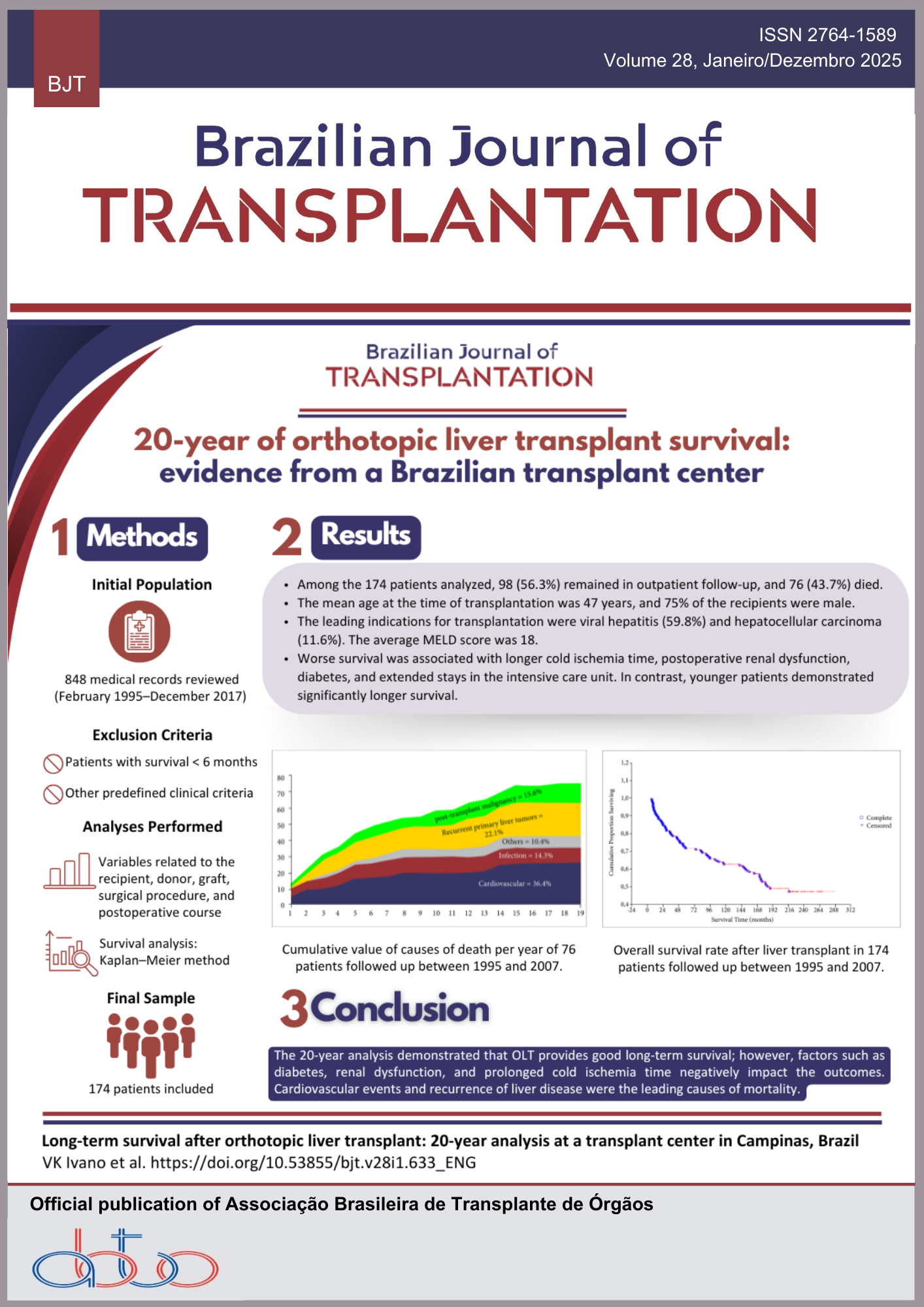
Sodium-Glucose Cotransporter 2 Inhibitors in Diabetic Kidney Transplant Recipients: Impact on Glycemic Control, Graft Function, and Proteinuria
Keywords:
Sodium-Glucose Transport Proteins, Diabetes Mellitus, Kidney Transplantation, Immunosuppressive agents, Graft SurvivalAbstract
Introduction: Sodium-glucose cotransporter 2 inhibitors (SGLT2i) improve albuminuria, the rate of chronic kidney disease (CKD) progression, and cardiovascular death in non-transplant patients with diabetes mellitus (DM) and proteinuria. However, kidney transplant recipients (KTRs) were excluded from the most extensive trials. This study aimed to evaluate graft function, proteinuria, and glycemic control in KTRs with pre- and post-transplant DM (PTDM) treated with SGLT2i. Methods: This is a single-center, retrospective, and observational study including transplant recipients older than 18 years old at transplantation, diagnosed with pre-transplant type 2 DM or PTDM, who were treated with SGLT2i after transplantation from June 2020 to June 2024. Results: Out of 1,883 KTRs followed at the center from June 2020 to June 2024, 31 patients received SGLT2i, 14 (45.2%) with pre-transplant DM, and 17 (54.8%) with PTDM. Fourteen (45.2%) completed the 24-month follow-up, including eight (57.1%) in the pre-transplant DM group and six (42.8%) in the PTDM group. In the pre-transplant DM group, fasting blood glucose (FBG) (134 [92-295] mg/dL vs. 109 [73-207], p = 0.24), estimated glomerular filtration rate (eGFR) (59.3 ± 19.2 vs. 68.1 ± 23.4, p = 0.35), and urinary protein-to-creatinine ratio (UPCR) (0.3 [0.0-1.9] vs. 0.3 [0.1-0.7], p = 0.80) remained stable. In the PTDM group, there was also no difference in the parameters analyzed, whether FBG (113 [95-225] mg/dL vs. 108 [92-149], p = 0.38), eGFR (73.1 ± 26.8 vs. 69.1 ± 28.9, p = 0.76), or UPCR (0.2 [0.1-2.5] vs. 0.2 [0.1-0.4], p = 0.21). Conclusion: These results suggest that the treatment has a beneficial effect on preserving graft function over a 2-year follow-up period. The treatment was well tolerated, with a low incidence of urinary tract infection or graft dysfunction.
Downloads
References
1. Koye DN, Magliano DJ, Nelson RG, Pavkov ME. The global epidemiology of diabetes and kidney disease. Adv Chronic Kidney Dis, 2018; 25(2): 121-32. https://doi.org/10.1053/j.ackd.2017.10.011
2. Rossi MR, Mazzali M, de Sousa MV. Oral glucose tolerance test as a risk marker for developing post transplant diabetes mellitus. Transplant Proc, 2024; 56(5): 1061-5. https://doi.org/10.1016/j.transproceed.2024.04.021
3. Chakkera HA, Weil EJ, Pham PT, Pomeroy J, Knowler WC. Can new-onset diabetes after kidney transplant be prevented? Diabetes Care, 2013; 36(5): 1406-12. https://doi.org/10.2337/dc12-2067
4. Paek JH, Kang SS, Park WY, Jin K, Park SB, Han S, et al. Incidence of post-transplantation diabetes mellitus within 1 year after kidney transplantation and related factors in Korean cohort study. Transplant Proc, 2019; 51(8): 2714-7. https://doi.org/10.1016/j.transproceed.2019.02.054
5. Rossi MR, Mazzali M, de Sousa MV. Post-transplant diabetes mellitus: risk factors and outcomes in a 5 year follow-up. Front Clin Diabetes Healthc, 2024; 5. https://doi.org/10.3389/fcdhc.2024.1336896
6. Birdwell KA, Park M. Post-transplant cardiovascular disease. Clin J Am Soc Nephrol, 2021; 16(12): 1878-89. https://doi.org/10.2215/CJN.00520121
7. Rodríguez-Rodríguez AE, Porrini E, Hornum M, Donate-Correa J, Morales-Febles R, Khemlani Ramchand S, et al. Posttransplant diabetes mellitus and prediabetes in renal transplant recipients: an update. Nephron, 2021; 145(4): 317-29. https://doi.org/10.1159/000514288
8. Lin H, Yan J, Yuan L, Qi B, Zhang Z, Zhang W, et al. Impact of diabetes mellitus developing after kidney transplantation on patient mortality and graft survival: a meta-analysis of adjusted data. Diabetol Metab Syndr, 2021; 13(1): 126. https://doi.org/10.1186/s13098-021-00742-4
9. Heerspink HJL, Kosiborod M, Inzucchi SE, Cherney DZI. Renoprotective effects of sodium-glucose cotransporter-2 inhibitors. Kidney Int, 2018; 94(1): 26-39. https://doi.org/10.1016/j.kint.2017.12.027
10. Montada-Atin T, PrasadGVR. Recent advances in new-onset diabetes mellitus after kidney transplantation. World J Diabetes, 2021; 12(5): 541-55. https://doi.org/10.4239/wjd.v12.i5.541
11. Pollock C, Stefánsson B, Reyner D, Rossing P, Sjöström CD, Wheeler DC, et al. Albuminuria-lowering effect of dapagliflozin alone and in combination with saxagliptin and effect of dapagliflozin and saxagliptin on glycaemic control in patients with type 2 diabetes and chronic kidney disease (DELIGHT): a randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol, 2019; 7(6): 429-41. https://doi.org/10.1016/S2213-8587(19)30086-5
12. Heerspink HJL, Stefánsson BV, Correa-Rotter R, Chertow GM, Greene T, Hou FF, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med, 2020; 383(15): 1436-46. https://doi.org/10.1056/NEJMoa2024816
13. Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med, 2019; 380(24): 2295-306. https://doi.org/10.1056/NEJMoa1811744
14. Suijk DLS, van Baar MJB, van Bommel EJM, Iqbal Z, Krebber MM, Vallon V, et al. SGLT2 inhibition and uric acid excretion in patients with type 2 diabetes and normal kidney function. Clin J Am Soc Nephrol, 2022; 17(5): 663-71. https://doi.org/10.2215/CJN.11480821
15. Mahling M, Schork A, Nadalin S, Fritsche A, Heyne N, Guthoff M. Sodium-glucose cotransporter 2 (SGLT2) inhibition in kidney transplant recipients with diabetes mellitus. Kidney Blood Press Res, 2019; 44(5): 984-92. https://doi.org/10.1159/000501854
16. Heerspink HJL, Perco P, Mulder S, Leierer J, Hansen MK, Heinzel A, et al. Canagliflozin reduces inflammation and fibrosis biomarkers: a potential mechanism of action for beneficial effects of SGLT2 inhibitors in diabetic kidney disease. Diabetologia, 2019; 62(7): 1154-66. https://doi.org/10.1007/s00125-019-4859-4
17. McGill JB, Subramanian S. Safety of sodium-glucose co-transporter 2 inhibitors. Am J Cardiol, 2019; 124: S45-52. https://doi.org/10.1016/j.amjmed.2019.08.006
18. Francis RS. SGLT2i after kidney transplantation: ready for prime time? Transplantation, 2022; 106(9): 1732-3. https://doi.org/10.1097/TP.0000000000004227
19. Lim JH, Kwon S, Jeon Y, Kim YH, Kwon H, Kim YS, et al. The efficacy and safety of SGLT2 inhibitors in diabetic kidney transplant recipients. Transplantation, 2022; 106(9): e404-12. https://doi.org/10.1097/TP.0000000000004228
20. Schwaiger E, Burghart L, Signorini L, Ristl R, Kopecky C, Tura A, et al. Empagliflozin in posttransplantation diabetes mellitus: a prospective, interventional pilot study on glucose metabolism, fluid volume, and patient safety. Am J Transplant, 2019; 19(3): 907-19. https://doi.org/10.1111/ajt.15223
21. Halden TAS, Kvitne KE, Midtvedt K, Rajakumar L, Robertsen I, Brox J, et al. Efficacy and safety of empagliflozin in renal transplant recipients with posttransplant diabetes mellitus. Diabetes Care, 2019; 42(6): 1067-74. https://doi.org/10.2337/dc19-0093
22. Shah M, Virani Z, Rajput P, Shah B. Efficacy and safety of canagliflozin in kidney transplant patients. Indian J Nephrol, 2019; 29(4): 278-81. https://doi.org/10.4103/ijn.IJN_2_18
23. Sánchez Fructuoso AI, Bedia Raba A, Banegas Deras E, Vigara Sánchez LA, Valero San Cecilio R, Franco Esteve A, et al. Sodium-glucose cotransporter-2 inhibitor therapy in kidney transplant patients with type 2 or post-transplant diabetes: an observational multicentre study. Clin Kidney J, 2023; 16(6): 1022-34. https://doi.org/10.1093/ckj/sfad007
24. Agarwal R. Pathogenesis of diabetic nephropathy. ADA Clinical Compendia, 2021; 2021(1) :2-7. https://doi.org/10.2337/db20211-2
25. Attallah N, Yassine L. Use of empagliflozin in recipients of kidney transplant: a report of 8 cases. Transplant Proc, 2019; 51(10): 3275-80. https://doi.org/10.1016/j.transproceed.2019.05.023
26. Ujjawal A, Schreiber B, Verma A. Sodium-glucose cotransporter-2 inhibitors (SGLT2i) in kidney transplant recipients: what is the evidence? Ther Adv Endocrinol Metab, 2022; 13. https://doi.org/10.1177/20420188221090001
27. AlKindi F, Al-Omary HL, Hussain Q, Al Hakim M, Chaaban A, Boobes Y. Outcomes of SGLT2 inhibitors use in diabetic renal transplant patients. Transplant Proc, 2020; 52(1): 175-8. https://doi.org/10.1016/j.transproceed.2019.11.007
28. Oliveras L, Montero N, Cruzado JM. Searching in the maze: sodium-glucose cotransporter-2 inhibitors in kidney transplant recipients to improve survival. Clin Kidney J, 2023; 16(6): 909-13. https://doi.org/10.1093/ckj/sfad045
29. Gibson C, Mount R, Valentine H, Sullivan D. Weight change in kidney transplant recipients: an academic medical centerbased study. Curr Dev Nutr, 2020; 4:nzaa063_035. https://doi.org/10.1093/cdn/nzaa063_035
30. Vallon V, Verma S. Effects of SGLT2 inhibitors on kidney and cardiovascular function. Annu Rev Physiol, 2021; 83(1): 503-28. https://doi.org/10.1146/annurev-physiol-031620-095920
31. Chewcharat A, Prasitlumkum N, Thongprayoon C, Bathini T, Medaura J, Vallabhajosyula S, et al. Efficacy and safety of SGLT-2 inhibitors for treatment of diabetes mellitus among kidney transplant patients: a systematic review and meta-analysis. Med Sci, 2020; 8(4): 47. https://doi.org/10.3390/medsci8040047
32. Lemke A, Brokmeier HM, Leung SB, Mara KC, Mour GK, Wadei HM, et al. Sodium-glucose cotransporter 2 inhibitors for treatment of diabetes mellitus after kidney transplantation. Clin Transplant, 2022; 36(8): e14718. https://doi.org/10.1111/ctr.14718
33. Polychronopoulou E, Bourdon F, Teta D. SGLT2 inhibitors in diabetic and non-diabetic kidney transplant recipients: current knowledge and expectations. Front Nephrol, 2024; 4. https://doi.org/10.3389/fneph.2024.1332397
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Matheus Rizzato Rossi, Leticia Harumi Richter Kawai , Marilda Mazzali, Marcos Vinícius de Sousa

This work is licensed under a Creative Commons Attribution 4.0 International License.