Construction and Validation of a Bundle for Screening and Diagnosis of Posttransplant Diabetes Mellitus in Kidney Transplant Recipients
Keywords:
Posttransplant Diabetes Mellitus, Kidney Transplant, Diagnosis, Clinical Protocols, Validation StudyAbstract
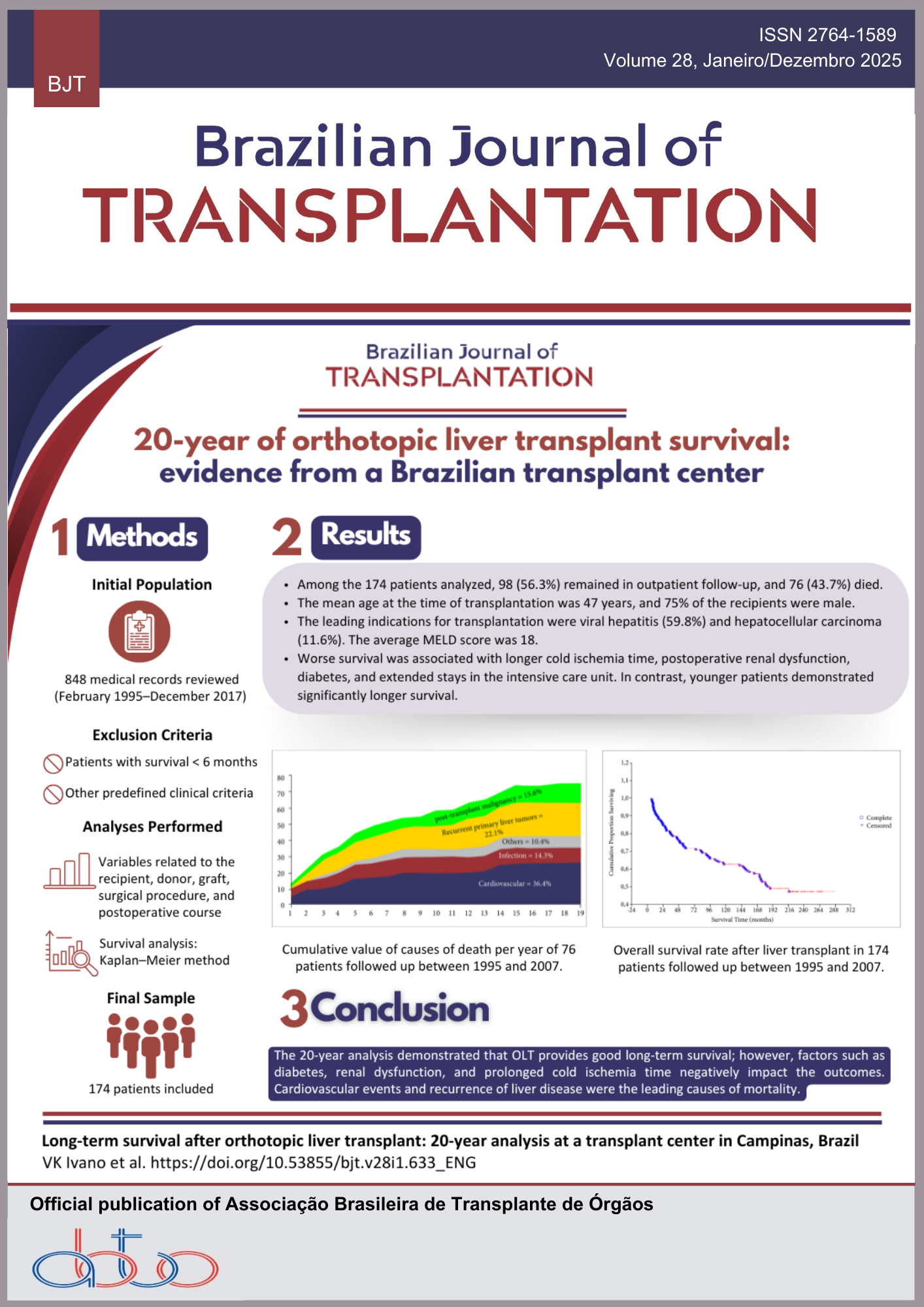
Introduction: Posttransplant diabetes mellitus (PTDM) is a potential consequence of kidney transplantation (KTx), and its prompt identification has a beneficial effect on patient longevity and graft maintenance. Although the diagnostic standards for PTDM remain identical to those used for the general public, the reliability of the assessments differs in KTx patients, and their recognition is often overlooked when fasting glucose (FG) is utilized as the sole screening method. Objectives: We intended to design and authenticate a care bundle for the screening and identification of PTDM in KTx individuals. Methods: The following procedures were carried out: a) literature survey; b) development of the bundle; and c) expert validation by qualified reviewers. The integrative review served as a resource in formulating the bundle. We assessed the experts’ feedback using the content validity index (CVI). A binomial analysis was executed to determine the consensus among the reviewers. Results: The bundle was organized to deliver guidance regarding: 1) which examination(s) to order; 2) the optimal timing to request them to distinguish PTDM from temporary hyperglycemia; and 3) which individuals require further assessments beyond FG. Every component was deemed validated, with an overall CVI of 0.99. Conclusion: The bundle was judged reliable for supporting clinical judgment in conducting PTDM screening and diagnosis in KTx individuals in a straightforward and efficient manner. We propose integrating this instrument into clinical routines due to its ease of use, affordability, and potential to enhance the care of these patients.
Downloads
References
1. Eide IA, Halden TAS, Hartmann A, Dahle DO, Åsberg A, Jenssen T. Associations between posttransplantation diabetes mellitus and renal graft survival. Transplantation. 2017; 101(6): 1282-9. https://doi.org/10.1097/TP.0000000000001259
2. Chevallier E, Jouve T, Rostaing L, Malvezzi P, Noble J. Pre-existing diabetes and PTDM in kidney transplant recipients: how to handle immunosuppression. Expert Rev Clin Pharmacol. 2021; 14(1): 55-66. https://doi.org/10.1080/17512433.2021.1851596
3. Jenssen T, Hartmann A. Post-transplant diabetes mellitus in patients with solid organ transplants. Nat Rev Endocrinol. 2019; 15(3): 172-88. https://doi.org/10.1038/s41574-018-0137-7
4. Conte C, Secchi A. Post-transplantation diabetes in kidney transplant recipients: an update on management and prevention. Acta Diabetol. 2018; 55(8): 763-79. https://doi.org/10.1007/s00592-018-1137-8
5. Caillard S, Eprinchard L, Perrin P, Braun L, Heibel F, Moreau F, et al. Incidence and risk factors of glucose metabolism disorders in kidney transplant recipients: role of systematic screening by oral glucose tolerance test. Transplantation. 2011; 91(7): 757-64. https://doi.org/10.1097/TP.0b013e31820f0877
6. Armstrong KA, Prins JB, Beller EM, Campbell SB, Hawley CM, Johnson DW, et al. Should an oral glucose tolerance test be performed routinely in all renal transplant recipients? Clin J Am Soc Nephrol. 2006; 1(1): 100-8. https://doi.org/10.2215/CJN.00090605
7. Shivaswamy V, Boerner B, Larsen J. Post-transplant diabetes mellitus: causes, treatment, and impact on outcomes. Endocr Rev. 2016; 37(1): 37-61. https://doi.org/10.1210/er.2015-1084
8. Resar R, Griffin FA, Haraden C, Nolan TW. Using care bundles to improve health care quality [Internet]. Cambridge: Institute for Healthcare Improvement; 2012. [cited 07 Aug 2021] Available from: http://www.ihi.org/resources/Pages/IHIWhitePapers/UsingCareBundles.aspx
9. Schünemann HJ, Wiercioch W, Etxeandia I, Falavigna M, Santesso N, Mustafa R,et al. Guidelines 2.0: systematic development of a comprehensive checklist for a successful guideline enterprise. Can Med Assoc J. 2014; 18; 186(3): E123-42. https://doi.org/10.1503/cmaj.131237
10. da Costa Santos CM, de Mattos Pimenta CA, Nobre MR. The PICO strategy for the research question construction and evidence search. Rev Lat Am Enfermagem. 2007; 15(3): 508-11. https://doi.org/10.1590/s0104-11692007000300023
11. Melnyk BM, Fineout-Overholt E. Evidence-based practice in nursing & healthcare: a guide to best practice. Philadelphia: Lippincott Williams & Wilkins; 2011.
12. Joventino ES. Construção e validação de escala para mensurar a autoeficácia materna na prevenção da diarreia infantil. Fortaleza. Dissertação [Mestrado em Enfermagem] – Universidade Federal do Ceará; 2010. http://repositorio.ufc.br/handle/riufc/1796
13. Teixeira E, Mota VMSS. Educação em saúde: tecnologias educacionais em foco. São Caetano do Sul: Difusão Editora; 2011.
14. Alexandre NMC, Coluci MZO. Validade de conteúdo nos processos de construção e adaptação de instrumentos de medidas. Ciênc. saúde coletiva. 2011; 16: 3061-8. https://doi.org/10.1590/S1413-81232011000800006
15. Polit DF, Beck CT. The content validity index: are you sure you know what’s being reported? Critique and recommendations. Res Nurs Health. 2006; 29(5): 489-97. https://doi.org/10.1002/nur.20147
16. Lopes MV de O, Silva VM da, Araújo TL de. Validação de diagnósticos de enfermagem: desafios e alternativas. Rev Bras Enferm. 2013; 66: 649-55. https://doi.org/10.1590/s0034-71672013000500002
17. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016; 15(2): 155-63. Erratum in: J Chiropr Med. 2017;16(4):346. https://doi.org/10.1016/j.jcm.2016.02.012
18. Kuypers DR, Claes K, Bammens B, Evenepoel P, Vanrenterghem Y. Early clinical assessment of glucose metabolism in renal allograft recipients: diagnosis and prediction of post-transplant diabetes mellitus (PTDM). Nephrol Dial Transplant. 2008; 23(6): 2033-42. https://doi.org/10.1093/ndt/gfm875
19. Valderhaug TG, Jenssen T, Hartmann A, Midtvedt K, Holdaas H, Reisaeter AV, et al. Fasting plasma glucose and glycosylated hemoglobin in the screening for diabetes mellitus after renal transplantation. Transplantation. 2009; 88(3): 429-34. https://doi.org/10.1097/TP.0b013e3181af1f53
20. Tatar E, Kircelli F, Demirci MS, Turan MN, Gungor O, Asci G, et al. Pre-transplant HbA1c level as an early marker for newonset diabetes after renal transplantation. Int Urol Nephrol. 2013; 45(1): 251-8. https://doi.org/10.1007/s11255-012-0304-z
21. Shabir S, Jham S, Harper L, Ball S, Borrows R, Sharif A. Validity of glycated haemoglobin to diagnose new onset diabetes after transplantation. Transpl Int. 2013; 26(3): 315-21. https://doi.org/10.1111/tri.12042
22. Yates CJ, Fourlanos S, Colman PG, Cohney SJ. Screening for new-onset diabetes after kidney transplantation: limitations of fasting glucose and advantages of afternoon glucose and glycated hemoglobin. Transplantation. 2013; 96(8): 726-31. https://doi.org/10.1097/TP.0b013e3182a012f3
23. Tokodai K, Amada N, Haga I, Nakamura A, Kashiwadate T, Kawagishi N, et al. Pretransplant HbA1c is a useful predictor for the development of new-onset diabetes in renal transplant recipients receiving no or low-dose erythropoietin. Int J Endocrinol. 2014; 2014: 436725. https://doi.org/10.1155/2014/436725
24. Tokodai K, Amada N, Haga I, Takayama T, Nakamura A. The 5-time point oral glucose tolerance test as a predictor of new-onset diabetes after kidney transplantation. Diabetes Res Clin Pract. 2014; 103(2): 298-303. https://doi.org/10.1016/j.diabres.2013.12.049
25. Clayton PA, Aouad L, Wyburn KR, Eris JM, Chadban SJ. HbA1c is insensitive at month 3 after kidney transplantation. Transplantation. 2015; 99(5): e37-8. https://doi.org/10.1097/TP.0000000000000683
26. Eide IA, Halden TA, Hartmann A, Åsberg A, Dahle DO, Reisæter AV, et al. Limitations of hemoglobin A1c for the diagnosis of posttransplant diabetes mellitus. Transplantation. 2015; 99(3): 629-35. https://doi.org/10.1097/TP.0000000000000376
27. Pimentel AL, Carvalho LS, Marques SS, Franco RF, Silveiro SP, Manfro RC, et al. Role of glycated hemoglobin in the screening and diagnosis of posttransplantation diabetes mellitus after renal transplantation: a diagnostic accuracy study. Clin Chim Acta. 2015; 445: 48-53. https://doi.org/10.1016/j.cca.2015.03.016
28. Rosettenstein K, Viecelli A, Yong K, Nguyen HD, Chakera A, Chan D, et al. Diagnostic accuracies of glycated hemoglobin, fructosamine, and homeostasis model assessment of insulin resistance in predicting impaired fasting glucose, impaired glucose tolerance, or new onset diabetes after transplantation. Transplantation. 2016; 100(7): 1571-9. https://doi.org/10.1097/TP.0000000000000949
29. Shin JI, Palta M, Djamali A, Astor BC. Higher pretransplantation hemoglobin A1c is associated with greater risk of posttransplant diabetes mellitus. Kidney Int Rep. 2017; 2(6): 1076-87. https://doi.org/10.1016/j.ekir.2017.06.006
30. Hap K, Madziarska K, Zmonarski S, Kamińska D, Magott-Procelewska M, Banasik M, et al. Pretransplantation oral glucose tolerance test can prevent posttransplant diabetes mellitus after renal transplantation: preliminary study. Transplant Proc. 2018; 50(6): 1776-80. https://doi.org/10.1016/j.transproceed.2018.03.125
31. Rao N, Rathi M, Sharma A, Ramachandran R, Kumar V, Kohli HS, et al. Pretransplant HbA1c and glucose metabolism parameters in predicting posttransplant diabetes mellitus and their course in the first 6 months after living-donor renal transplant. Exp Clin Transplant. 2018; 16(4): 446-54. https://doi.org/10.6002/ect.2017.0020
32. Tillmann FP, Rump LC, Quack I. HbA1c levels at 90 days after renal transplantation in non-diabetic recipients predict de novo pre-diabetes and diabetes at 1 and 3 years after transplantation. Int Urol Nephrol. 2018; 50(8): 1529-34. https://doi.org/10.1007/s11255-018-1917-7
33. Lai X, Zhang L, Fang J, Li G, Xu L, Ma J, et al. OGTT 2-hour serum C-peptide index as a predictor of post-transplant diabetes mellitus in kidney transplant recipients. Ann Transl Med. 2019; 7(20): 538. https://doi.org/10.21037/atm.2019.10.14
34. Ussif AM, Åsberg A, Halden TAS, Nordheim E, Hartmann A, Jenssen T. Validation of diagnostic utility of fasting plasma glucose and HbA1c in stable renal transplant recipients one year after transplantation. BMC Nephrol. 2019; 20(1): 12. https://doi.org/10.1186/s12882-018-1171-3
35. Pimentel AL, Hernandez MK, Freitas PAC, Chume FC, Camargo JL. The usefulness of glycated albumin for posttransplantation diabetes mellitus after kidney transplantation: a diagnostic accuracy study. Clin Chim Acta. 2020; 510: 330-6. https://doi.org/10.1016/j.cca.2020.07.045
36. Sharif A, Hecking M, de Vries AP, Porrini E, Hornum M, Rasoul-Rockenschaub S, et al. Proceedings from an international consensus meeting on posttransplantation diabetes mellitus: recommendations and future directions. Am J Transplant. 2014; 14(9): 1992-2000. https://doi.org/10.1111/ajt.12850
37. Rodríguez-Rodríguez AE, Porrini E, Hornum M, Donate-Correa J, Morales-Febles R, Khemlani Ramchand S, et al. Posttransplant diabetes mellitus and prediabetes in renal transplant recipients: an update. Nephron. 2021; 145(4): 317-29. https://doi.org/10.1159/000514288
38. Pimentel AL, Cavagnolli G, Camargo JL. Diagnostic accuracy of glycated hemoglobin for post transplantation diabetes mellitus after kidney transplantation: systematic review and meta-analysis. Nephrol Dial Transplant. 2017; 32(3): 565-72. https://doi.org/10.1093/ndt/gfw437
39. Adnan S, Harini C, Aiko PJV, Kathrin E, Martina G, Maria CH, et al. International consensus on post transplant diabetes mellitus. Nephrol Dial Transplant. 2024; 39(3): 531-49. https://doi.org/10.1093/ndt/gfad258
40. Ellie O, Peyton C, Marissa LO, Jared LO. Post-renal transplant diabetes mellitus. USA Pharm. 2023. 48(11): HS12-HS16. Available from: https://www.uspharmacist.com/article/diabetes-mellitus-post kidney-transplant
41. Bergman M, Manco M, Satman I, Chan J, Schmidt MI, Sesti G, et al. International Diabetes Federation position statement on the 1-hour post-load plasma glucose for the diagnosis of intermediate hyperglycaemia and type 2 diabetes. Diabetes Res Clin Pract. 2024; 209: 111589. https://doi.org/10.1016/j.diabres.2024.111589
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Tamizia Cristino Severo de Souza, Ivelise Regina Canito Brasil, Tainá Veras de Sandes Freitas, Elias Bruno Coelho Gouveia, Francisca Christina Silva Rabelo, Cristina Micheletto Dallago

This work is licensed under a Creative Commons Attribution 4.0 International License.