Admissions Within the First Year After Kidney Transplantation: Evaluation of Risk Factors, Causes, and Outcomes
Keywords:
Kidney Transplantation, Hospitalization, Opportunistic InfectionsAbstract
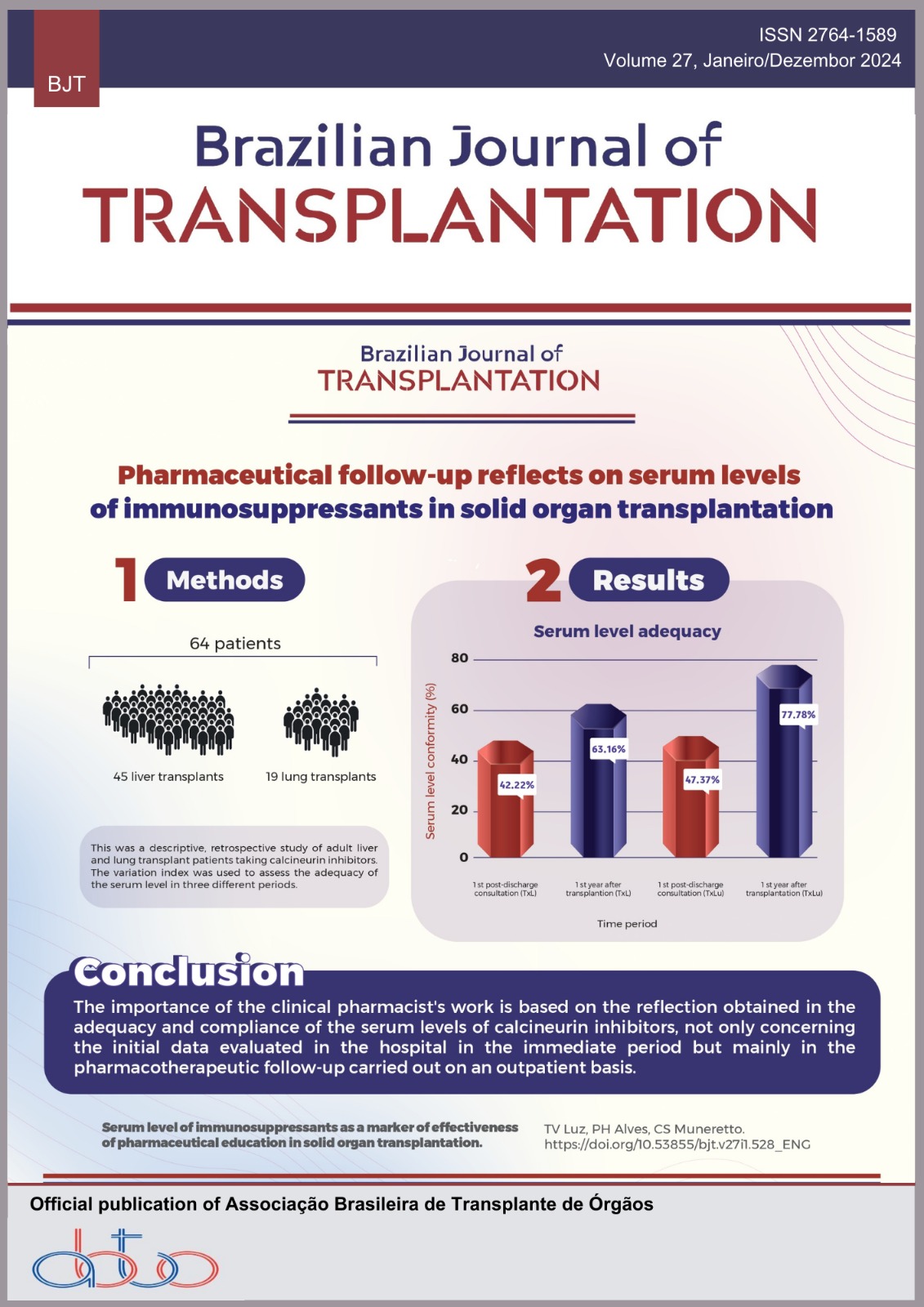
Objectives: The aim of this study was to evaluate causes of hospital admission within the 1st year after kidney transplantation in a public hospital. Methods: This is a retrospective cohort. Data were collected by medical record review. Inclusion criteria were age older than 18 years and kidney transplant. Exclusion criteria were double transplant, primary graft failure, and in-hospital death after transplant procedure. Outcomes included 4-year patient survival (primary outcome), 1-year graft failure, and graft function in 1 year. Results: A total of 130 patients were evaluated. There was a predominance of male sex, glomerulonephritis, history of hemodialysis, first kidney transplant, and deceased donor kidneys. Hospital admission in the 1st year occurred in 71.5%. There were three deaths at the first admission (two had cardiovascular causes). The most frequent causes of admission were infections, rejection, and surgical complications. Less common causes included elective procedures such as peritoneal dialysis catheter removal. There was no statistically significant association between categorical and continuous variables studied and the occurrence of hospital admission. Also, hospital admission did not influence primary outcome or 1-year graft failure rate. However, it was associated with lower graft function at 1 year (both by serum creatinine and by estimated glomerular filtration rate – p < 0.05). Conclusion: There was a high incidence of hospital admission, and first admissions resulted in death in three patients (noninfectious causes). Considering the contribution of elective procedures to the high incidence of admission, we propose that hospital managers focus on improving the ability to solve such problems in the outpatient setting.
Downloads
References
Abecassis M, Bartlett ST, Collins AJ, Davis CL, Delmonico FL, Friedewald JJ, et al. Kidney transplantation as primary therapy for end-stage renal disease: a National Kidney Foundation/Kidney Disease Outcomes Quality Initiative (NKF/KDOQI) conference. Clin J Am Soc Nephrol 2008; 3: 471-80. https://doi.org/10.2215/CJN.05021107
Schnuelle P, Lorenz D, Trede M, Van der Woude FJ. Impact of renal cadaveric transplantation on survival in end-stage renal failure: evidence for reduced mortality risk compared with hemodialysis during long-term follow-up. J Am Soc Nephrol 1998; 9: 2135-41. https://doi.org/10.1681/ASN.V9112135
Ojo AO, Port FK, Wolfe RA, Mauger EA, Williams L, Berling DP. Comparative mortality risks of chronic dialysis and cadaveric transplantation in black end-stage renal disease patients. Am J Kidney Dis 1994; 24: 59-64. https://doi.org/10.1016/ S0272-6386(12)80160-0
Rabbat CG, Thorpe KE, Russell JD, Churchill DN. Comparison of mortality risk for dialysis patients and cadaveric first renal transplant recipients in Ontario, Canada. J Am Soc Nephrol 2000; 11: 917-22. https://doi.org/10.1681/ASN.V115917
Teixeira JP, Combs SA, Teitelbaum I. Peritoneal dialysis: update on patient survival. Clin Nephrol 2015; 83: 1-10. https://doi.org/10.5414/CN108382
Sukul N, Mukhopadhyay P, Schaubel DE, Pearson J, Turenne M, Saran R, et al. Peritoneal dialysis and mortality, kidney transplant, and transition to hemodialysis: trends from 1996-2015 in the United States. Kidney Med; 2: 610-9. https://doi.org/10.1016/j.xkme.2020.06.009
Port FK, Wolfe RA, Mauger EA, Berling DP, Jiang K. Comparison of survival probabilities for dialysis patients vs cadaveric renal transplant recipients. J Am Med Assoc 1993; 270: 1339-43. https://doi.org/10.1001/jama.1993.03510110079036
United States Renal Data System [homepage na Internet]. Annual Data Report: mortality and causes of death [Atualizado em: Nov 2019, accessado em: Ago 22 2022]. Available from:www.usrds.org/annual-data-report/
Boenink R, Stel VS, Waldum-Grevbo BE, Collart F, Kerschbaum J, Heaf JG, et al. Data from the ERA-EDTA Registry was examined for trends in excess mortality in European adults on kidney replacement therapy. Kidney Int 2020; 98: 999-1008. https://doi.org/10.1016/j.kint.2020.05.039
Ying T, Shi B, Kelly PJ, Pilmore H, Clayton PA, Chadban SJ. Death after kidney transplantation: an analysis by era and time post-transplant. J Am Soc Nephrol 2020; 31: 2887-99. https://doi.org/10.1681/ASN.2020050566
Yagisawa T, Mieno M, Ichimaru N, Morita K, Nakamura M, Hotta K, et al. Trends of kidney transplantation in Japan in 2018: data from the kidney transplant registry. Ren Replace Ther 2019;5:1-14. https://doi.org/10.1186/s41100-019-0199-6
United States Renal Data System [homepage na Internet]. 2019 USRDS Annual Data Report: epidemiology of kidney disease in the United States [Atualizado em: Nov 2019; Acessado em: Ago 22 2022]. Available from:https://www.usrds.org/annual-data-report/
Schmidt-Lauber C, Günster C, Huber TB, Spoden M, Grahammer F. Collateral effects and mortality of kidney transplant recipients during the COVID-19 pandemic. Kidney360 2022; 3: 325-36. https://doi.org/10.34067/KID.0006472021
Requião-Moura LR, Sandes-Freitas TV, Viana LA, Cristelli MP, Andrade LGM, Garcia VD, et al. High mortality among kidney transplant recipients diagnosed with coronavirus disease 2019: results from the Brazilian multicenter cohort study. PLoS ONE 2021; 16: 1-20. https://doi.org/10.1371/journal.pone.0254822
Farrugia D, Cheshire J, Begaj I, Khosla S, Ray D, Sharif A. Death within the first year after kidney transplantation: an observational cohort study. Transpl Int 2014; 27: 262-70. https://doi.org/10.1111/tri.12218
Prihodova L, Nagyova I, Rosenberger J, Majernikova M, Roland R, Groothoff JW, et al. Adherence in patients in the first year after kidney transplantation and its impact on graft loss and mortality: a cross-sectional and prospective study. J Adv Nurs 2014; 70: 2871-83. https://doi.org/10.1111/jan.12447
Tavares MG, Tedesco-Silva Junior H, Pestana JOM. Readmissão hospitalar precoce no transplante renal: artigo de revisão. J Bras Nefrol 2020; 42: 231-7. https://doi.org/10.1590/2175-8239-JBN-2019-0089
Pestana JM. A pioneering healthcare model applying large-scale production concepts: principles and performance after more than 11,000 transplants at Hospital do Rim. Rev Assoc Med Bras 2016; 62: 664-71. https://doi.org/10.1590/1806- 9282.62.07.664
Boubaker K, Harzallah A, Ounissi M, Becha M, Guergueh T, Hedri H. Rehospitalization after kidney transplantation during the first year: length, causes and relationship with long-term patient and graft survival. Transplant Proc 2011; 43: 1742-6. https://doi.org/10.1016/j.transproceed.2011.01.178
Nguyen MC, Avila CL, Brock GN, Benedict JA, James I, El-Hinnawy A, et al. "Early" and "late" hospital readmissions in the first year after kidney transplant at a single center. Clin Transplant 2020; 34: 1-11. https://doi.org/10.1111/ctr.13822
Kim SH, Baird GL, Bayliss G, Merhi B, Osband A, Gohh R, et al. A single-center analysis of early readmission after renal transplantation. Clin Transplant 2019; 33: 1-6. https://doi.org/10.1111/ctr.13520
Weeda ER, Su Z, Taber DJ, Bian J, Morinelli TA, Pilch NA, et al. Hospital admissions and emergency department visits among kidney transplant recipients. Clin Transplant 2019; 33: e13522. https://doi.org/10.1111/ctr.13522
Wongtanasarasin W, Phinyo P. Emergency department visits and hospital admissions in kidney transplant recipients during the COVID-19 pandemic: a hospital-based study. World J Transplant 2022;12: 250-8. https://doi.org/10.5500/wjt.v12.i8.250
Tavares MG, Cristelli MP, Paula MI, Viana L, Felipe CR, Proença H, et al. Early hospital readmission after kidney transplantation under a public health care system. Clin Transplant 2019; 33: e13467. https://doi.org/10.1111/ctr.13467
Tavares MG, Cristelli MP, Taddeo J, Tedesco-Silva Junior H, Pestana JM. The impact of universal induction therapy on early hospital readmission of kidney transplant recipients. Braz J Nephrol 2023; 45: 218-28. https://doi.org/10.1590%2F2175-8239-JBN-2022-0042en
Luan FL, Barrantes F, Roth RS, Samaniego M. Early hospital readmissions post-kidney transplantation are associated with inferior clinical outcomes. Clin Transplant 2014; 28: 487-93. https://doi.org/10.1111/ctr.12347
Lubetzky M, Yaffe H, Chen C, Ali H, Kayler LK. Early readmission after kidney transplantation: examination of discharge- level factors. Transplantation 2016; 100: 1079-85. https://doi.org/10.1097/tp.0000000000001089
McAdams-DeMarco MA, Grams ME, Hall EC, Coresh J, Segev DL. Early hospital readmission after kidney transplantation: patient and center-level associations. Am J Transplant 2012; 12: 3283-8. https://doi.org/10.1111/j.1600-6143.2012.04285.x
Kang IC, Kim IK, Son S, Ju MK. Impact of early hospital readmissions after kidney transplantation on graft function. Transplant Proc 2017; 50: 2359-62. https://doi.org/10.1016/j.transproceed.2017.12.062
Famure O, Kim ED, Li Y, Huang JW, Zyla R, Au M, et al. Outcomes of early hospital readmission after kidney transplantation: perspectives from a Canadian transplant centre. World J Transplant 2023; 13: 357-67. https://doi.org/10.5500/wjt.v13.i6.357
King EA, Bowring MG, Massie AB, Kucirka LM, McAdams-DeMarco MA, Al-Ammary F, et al. Mortality and graft loss attributable to readmission after kidney transplantation: immediate and long-term risk. Transplantation 2017; 101: 2520-6. https://doi.org/10.1097/tp.0000000000001609
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Víctor Mendes Ferreira, Clarice de Carvalho Silva Sarcinelli, Andre de Sousa Alvarenga

This work is licensed under a Creative Commons Attribution 4.0 International License.