Diferenças de Gênero na COVID-19 entre Receptores de Transplante de Fígado: Resultados de uma Coorte Multicêntrica Brasileira
Palavras-chave:
Transplante Hepático, COVID-19, Necessidades Específicas de GêneroResumo
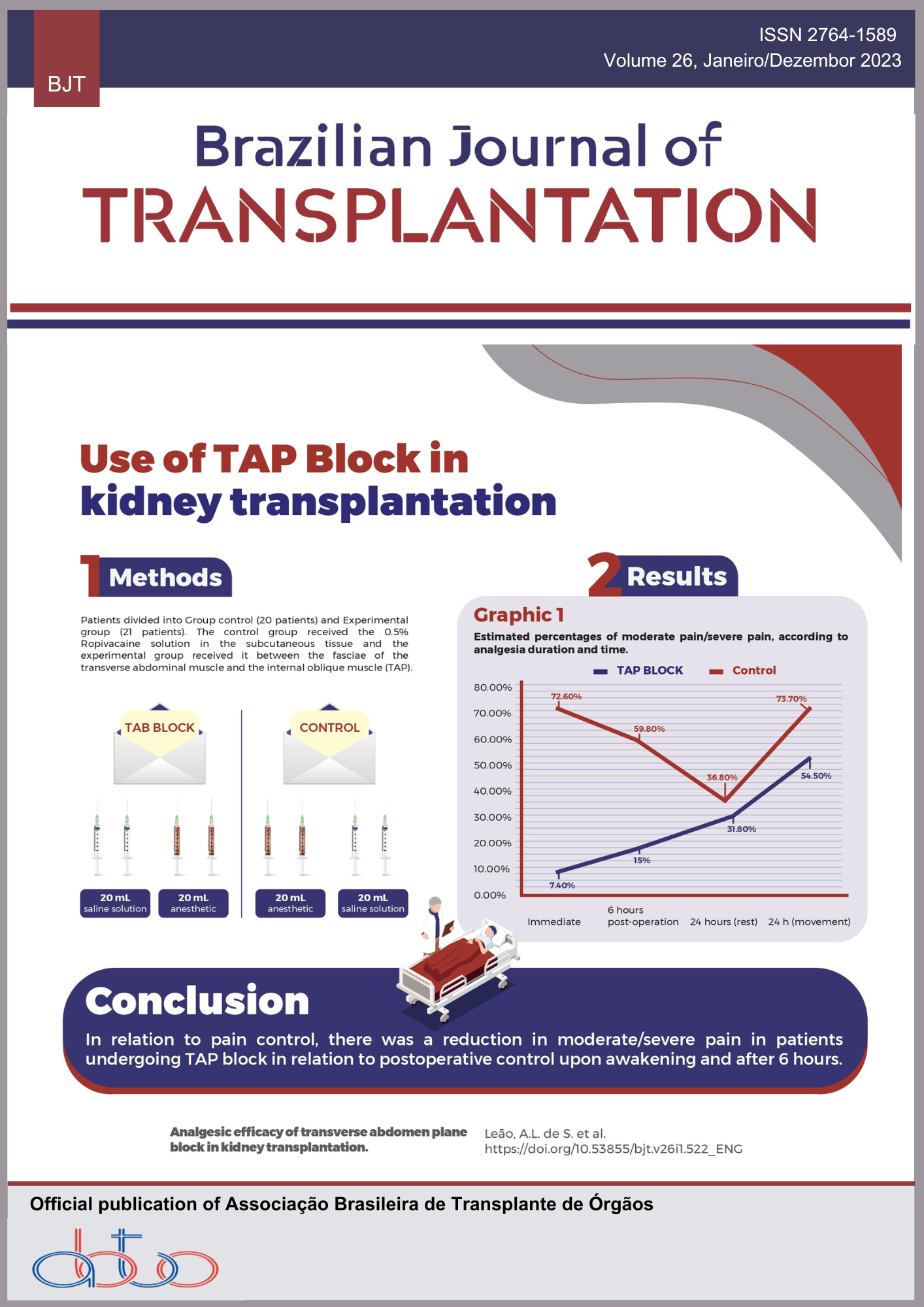
Introdução: A literatura existente apresenta perspectivas variadas sobre o impacto da COVID-19 em receptores de transplante de fígado. No entanto, nenhuma pesquisa investigou especificamente o papel das diferenças de gênero na manifestação da COVID-19 entre os receptores de transplante de fígado. Este estudo pretende examinar os efeitos da COVID-19 em receptores de transplante de fígado, com foco nas diferenças de gênero na apresentação e progressão da doença. Métodos: Conduzida como um estudo de coorte histórico multicêntrico, esta pesquisa coletou registros de pacientes por meio de um questionário on-line. O principal objetivo foi avaliar a mortalidade relacionada à COVID. Além disso, foram coletados dados demográficos, clínicos e laboratoriais relativos à apresentação e progressão da doença. Resultados: O estudo incluiu um total de 283 pacientes, sendo 76 do sexo feminino e 206 do sexo masculino. O período médio de acompanhamento para os homens foi de 99 dias (IQR 38-283), enquanto para as mulheres foi de 126 dias (IQR 44-291). Foi observada uma maior prevalência de doença cardiovascular nos homens (p=0,002). As mulheres frequentemente apresentavam perda de olfato (p=0,021), enquanto os homens geralmente apresentavam febre (p=0,031). Os níveis de ALT e gama-glutamil transferase foram significativamente elevados nos homens (p=0,008 e 0,004, respectivamente). Embora tenha havido uma tendência de aumento da mortalidade nos homens, ela não alcançou significância estatística. Conclusão: Este estudo é a primeira tentativa de investigar as diferenças de gênero na COVID-19 entre os receptores de transplante de fígado. Nossos achados destacam a necessidade de uma abordagem abrangente e personalizada para tratar essa população de pacientes e ressaltam a importância de elucidar melhor a apresentação da doença nesses indivíduos.
Downloads
Referências
Kassas ME, Alboraie M, Balakosy AA, Abdeen N, Afify S, Abdalgaber M, et al. Liver transplantation in the era of COVID-19. Arab J Gastroenterol, 2020;21(2):69–75. https://doi.org/10.1016%2Fj.ajg.2020.04.019
Loinaz-Segurola C, Marcacuzco-Quinto A, Fernández-Ruiz M. Coronavirus disease 2019 in liver transplant patients: Clinical and therapeutic aspects. World Journal of Hepatology. 2021;13(10):1299–315. https://doi.org/10.4254%2Fwjh.v13.i10.1299
Maira TD, Berenguer M. COVID-19 and liver transplantation. Nat Rev Gastroenterol Hepatol. 2020;17(9):526–8. https://doi.org/10.1038/s41575-020-0347-z
Phipps MM, Verna EC. Coronavirus Disease 2019 and Liver Transplantation: Lessons from the First Year of the Pandemic. Liver Transpl. 2021;27(9):1312–25. https://doi.org/10.1002/lt.26194
Sahin TT, Akbulut S, Yilmaz S. COVID-19 pandemic: Its impact on liver disease and liver transplantation. World J Gastroenterol. 2020;26(22):2987–99. https://doi.org/10.3748%2Fwjg.v26.i22.2987
Kates OS, Haydel BM, Florman SS, Rana MM, Chaudhry ZS, Ramesh MS, et al. COVID-19 in solid organ transplant: A multi-center cohort study. Clin Infect Dis. 2020. https://doi.org/10.1093%2Fcid%2Fciaa1097
Pereira MR, Mohan S, Cohen DJ, Husain SA, Dube GK, Ratner LE, et al. COVID-19 in solid organ transplant recipients: Initial report from the US epicenter. Am J Transplant. 2020;20(7):1800–8. https://doi.org/10.1111/ajt.15941
Belli LS, Fondevila C, Cortesi PA, Conti S, Karam V, Adam R, et al. Protective Role of Tacrolimus, Deleterious Role of Age and Comorbidities in Liver Transplant Recipients With Covid-19: Results From the ELITA/ELTR Multi-center European Study. Gastroenterology. 2021;160(4):1151-1163.e3. https://doi.org/10.1053/j.gastro.2020.11.045
Belli LS, Duvoux C, Karam V, Adam R, Cuervas-Mons V, Pasulo L, et al. COVID-19 in liver transplant recipients: preliminary data from the ELITA/ELTR registry. The Lancet Gastroenterology & Hepatology. 2020;5(8):724–5. https://doi.org/10.1016/S2468-1253(20)30183-7
Coll E, Fernández-Ruiz M, Padilla M, Moreso F, Hernández-Vicente A, Yañez Í, et al. COVID-19 in Solid Organ Transplant Recipients in Spain Throughout 2020: Catching the Wave? Transplantation. 2021;105(10):2146–55. https://doi.org/10.1097/tp.0000000000003873
Coll E, Fernández-Ruiz M, Sánchez-Álvarez JE, Martínez-Fernández JR, Crespo M, Gayoso J, et al. COVID-19 in transplant recipients: The Spanish experience. Am J Transplant. 2021;21(5):1825–37. https://doi.org/10.1111/ajt.16369
Dumortier J, Duvoux C, Roux O, Altieri M, Barraud H, Besch C, et al. Covid-19 in liver transplant recipients: the French SOT COVID registry. Clin Res Hepatol Gastroenterol. 2021;45(4):101639. https://doi.org/10.1016/j.clinre.2021.101639
Miarons M, Larrosa-García M, García-García S, Los-Arcos I, Moreso F, Berastegui C, et al. COVID-19 in Solid Organ Transplantation: A Matched Retrospective Cohort Study and Evaluation of Immunosuppression Management. Transplantation. 2021;105(1):138–50. https://doi.org/10.1097/TP.0000000000003460
Webb GJ, Marjot T, Cook JA, Aloman C, Armstrong MJ, Brenner EJ, et al. Outcomes following SARS-CoV-2 infection in liver transplant recipients: an international registry study. The Lancet Gastroenterology & Hepatology. 2020;5(11):1008–16. https://doi.org/10.1016/S2468-1253(20)30271-5
Kulkarni AV, Tevethia HV, Premkumar M, Arab JP, Candia R, Kumar K, et al. Impact of COVID-19 on liver transplant recipients-A systematic review and meta-analysis. EClinicalMedicine. 2021;38:101025. https://doi.org/10.1016/j.eclinm.2021.101025
Mansoor E, Perez A, Abou-Saleh M, Sclair SN, Cohen S, Cooper GS, et al. Clinical Characteristics, Hospitalization, and Mortality Rates of Coronavirus Disease 2019 Among Liver Transplant Patients in the United States: A Multicenter Research Network Study. Gastroenterology. 2021;160(1):459-462.e1. https://doi.org/10.1053/j.gastro.2020.09.033
Ritchie H, Mathieu E, Rodés-Guirao L, Appel C, Giattino C, Ortiz-Ospina E, et al. Coronavirus Pandemic (COVID-19). 2020. Disponível em: https://ourworldindata.org/coronavirus
Rabinowich L, Grupper A, Baruch R, Ben-Yehoyada M, Halperin T, Turner D, et al. Low immunogenicity to SARS-CoV-2 vaccination among liver transplant recipients. J Hepatol. 2021;75(2):435–8. https://doi.org/10.1016/j.jhep.2021.04.020
Toniutto P, Falleti E, Cmet S, Cussigh A, Veneto L, Bitetto D, et al. Past COVID-19 and immunosuppressive regimens affect the long-term response to anti-SARS-CoV-2 vaccination in liver transplant recipients. J Hepatol. 2022;77(1):152–62. https://doi.org/10.1016/j.jhep.2022.02.015
Hardgrave H, Wells A, Nigh J, Klutts G, Krinock D, Osborn T, et al. COVID-19 Mortality in Vaccinated vs. Unvaccinated Liver & Kidney Transplant Recipients: A Single-Center United States Propensity Score Matching Study on Historical Data. Nato Adv Sci Inst Se. 2022;10(11):1921. https://doi.org/10.3390/vaccines10111921
Ma E, Ai J, Zhang Y, Zheng J, Gao X, Xu J, et al. Omicron infections profile and vaccination status among 1881 liver transplant recipients: a multi-centre retrospective cohort. Emerg Microbes Infec. 2022;11(1):2636–44. https://doi.org/10.1080%2F22221751.2022.2136535
Hamm SR, Rezahosseini O, Møller DL, Loft JA, Poulsen JR, Knudsen JD, et al. Incidence and severity of SARS-CoV-2 infections in liver and kidney transplant recipients in the post-vaccination era: Real-life data from Denmark. Am J Transplant. 2022;22(11):2637–50. https://doi.org/10.1111/ajt.17141
Su YJ, Kuo KC, Wang TW, Chang CW. Gender-based differences in COVID-19. New Microbes New Infect. 2021;42:100905. https://doi.org/10.1016/j.nmni.2021.100905
Ahmed MM, Sayed AM, Abd DE, Fares S, Said MSM, Ebrahim EES. Gender Difference in Perceived Symptoms and Laboratory Investigations in Suspected and Confirmed COVID-19 Cases: A Retrospective Study. J Prim Care Community Heal. 2021;12:215013272110397. https://doi.org/10.1177/21501327211039718
Ten-Caten F, Gonzalez-Dias P, Castro Í, Ogava RLT, Giddaluru J, Silva JCS, et al. In-depth Analysis of Laboratory Parameters Reveals the Interplay Between Sex, Age and Systemic Inflammation in Individuals with COVID-19. Int J Infect Dis Ijid Official Publ Int Soc Infect Dis. 2021;105:579–87. https://doi.org/10.1016/j.ijid.2021.03.016
Colmenero J, Rodríguez-Perálvarez M, Salcedo M, Arias-Milla A, Muñoz-Serrano A, Graus J, et al. Epidemiological pattern, incidence, and outcomes of COVID-19 in liver transplant patients. J Hepatol. 2021;74(1):148–55. https://doi.org/10.1016/j.jhep.2020.07.040
Liu H, He X, Wang Y, Zhou S, Zhang D, Zhu J, et al. Management of COVID-19 in patients after liver transplantation: Beijing working party for liver transplantation. Hepatol Int. 2020;14(4):432–6. https://doi.org/10.1007/s12072-020-10043-z
Hou Y, Zhou Y, Gack MU, Lathia JD, Kallianpur A, Mehra R, et al. Multimodal single-cell omics analysis identifies epithelium–immune cell interactions and immune vulnerability associated with sex differences in COVID-19. Signal Transduct Target Ther. 2021;6(1):292. https://doi.org/10.1038/s41392-021-00709-x
Rehman S, Ravinayagam V, Nahvi I, Aldossary H, Al-Shammari M, Amiri MSA, et al. Immunity, Sex Hormones, and Environmental Factors as Determinants of COVID-19 Disparity in Women. Front Immunol. 2021;12:680845. https://doi.org/10.3389/fimmu.2021.680845
Pereira MR, Arcasoy S, Farr MA, Mohan S, Emond JC, Tsapepas DS, et al. Outcomes of COVID-19 in solid organ transplant recipients: A matched cohort study. Transpl Infect Dis. 2021;23(4):e13637. https://doi.org/10.1097/tp.0000000000003670
Wang XW, Hu H, Xu ZY, Zhang GK, Yu QH, Yang HL, et al. Association of menopausal status with COVID-19 outcomes: a propensity score matching analysis. Biol Sex Differ. 2021;12(1):16. https://doi.org/10.1186/s13293-021-00363-6
Cai Z, Yang Y, Zhang J. Obesity is associated with severe disease and mortality in patients with coronavirus disease 2019 (COVID-19): a meta-analysis. Bmc Public Health. 2021;21(1):1505. https://doi.org/10.1186/s12889-021-11546-6
Gleeson LE, Roche HM, Sheedy FJ. Obesity, COVID-19 and innate immunometabolism. Brit J Nutr. 2020;125(6):628–32. https://doi.org/10.1017%2FS0007114520003529
Dessie ZG, Zewotir T. Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients. Bmc Infect Dis. 2021;21(1):855. https://doi.org/10.1186/s12879-021-06536-3
Downloads
Publicado
Como Citar
Edição
Seção
Licença
Copyright (c) 2023 Elaine Cristina Ataide, Eduardo Riccetto, Tercio Genzini, Regina Gomes Santos, Lucio F Pacheco Moreira, Laura Cristina Machado Pinto, Raquel S B Stucchi, Simone Reges Perales, Leticia Zanaga, Renato Ferreira da Silva, Rita C M Ferreira da Silva, Luciana Haddad, Luiz A C D´'Albuquerque, Marcio Dias de Almeida, Andre Watanabe, Gustavo S Peixoto, Claudio Moura Lacerda de Melo, Renata Ferreira, Nertan Luiz Tefilli, Marcia Halpern, Maira Silva Godoy, Marcelo Nogara, Jorge Marcelo Padilla Mancero, Huda Maria Noujaim, José Huygens Parente Garcia, Erika Bevilaqua Rangel, Ilka de Fátima Santana Ferreira Boin

Este trabalho está licenciado sob uma licença Creative Commons Attribution 4.0 International License.